Summary
Suicide is the leading cause of violent deaths in the U.S. and the second leading cause of all deaths for youth ages 10–24 (Centers for Disease Control and Prevention, 2019). However, the large majority of U.S. adults, including health care professionals, are unable to correctly identify the most common causes (suicide versus homicide) and means (firearms versus non-firearms) of violent deaths (Morgan et al., 2018). These misperceptions can hinder support and funding for suicide prevention as well as implementation of effective prevention strategies. The role of firearms in deaths by suicide is particularly important as they are the most lethal means available, with a lethality rate that is more than 80% compared to a lethality rate of under 2% for overdoses (Conner, Azrael, & Mille, 2019; Shenassa, Catlin, & Burka, 2003). Lethal means are objects (e.g., medications, firearms, knives) that are used to engage in suicide attempts, and lethal means safety counseling is one of the few evidence-based strategies found to significantly reduce suicide deaths (Zalsman et al., 2016). Lethal means safety counseling involves assessing whether a person at risk for suicide has access to lethal means and working with them and their support system to limit their access to those means in times of crisis. Given the lethality of firearms, the high rates of death by suicide among youth, and the importance of lethal means safety counseling as a suicide prevention strategy, it is imperative to examine lethal means in relation to deaths by suicide among youth. There is also a vital need for data on sexual orientation and gender identity to understand how lethal means impact deaths by suicide among LGBTQ youth. This research brief utilizes data from the Centers for Disease Control and Prevention (CDC’s) National Vital Statistics System to examine suicide deaths among U.S. youth ages 10–24.
Results
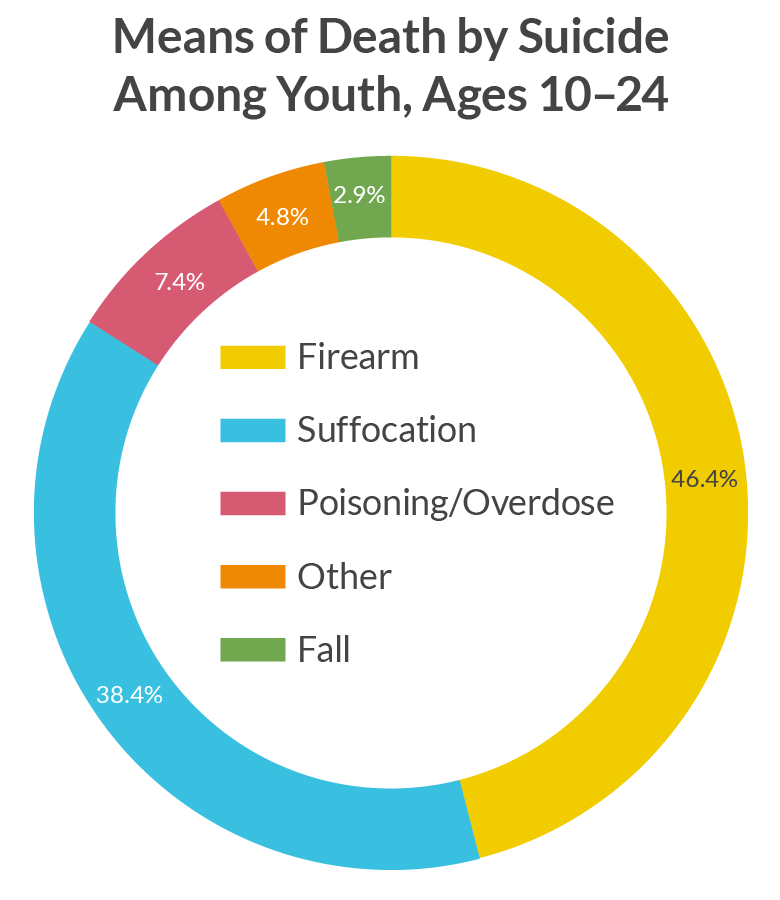
In 2017, firearms were the most common means of suicide deaths among youth ages 10–24 in the U.S., accounting for nearly half of all deaths by suicide. The proportion of suicides attributed to firearms were highest in the South (55%) compared to the Northeast (45%), Midwest (48%), and West (45%). Rates were also lower among youth ages 10–14 (39%), compared to those ages 15–19 (46%), and 20–24 (51%). White non-Hispanic (50%) and Black/African American (50%) youth were more likely to die by suicide using a firearm compared to American Indian/Alaskan Native (38%), Hispanic (37%), and Asian/Pacific Islander (30%) youth.
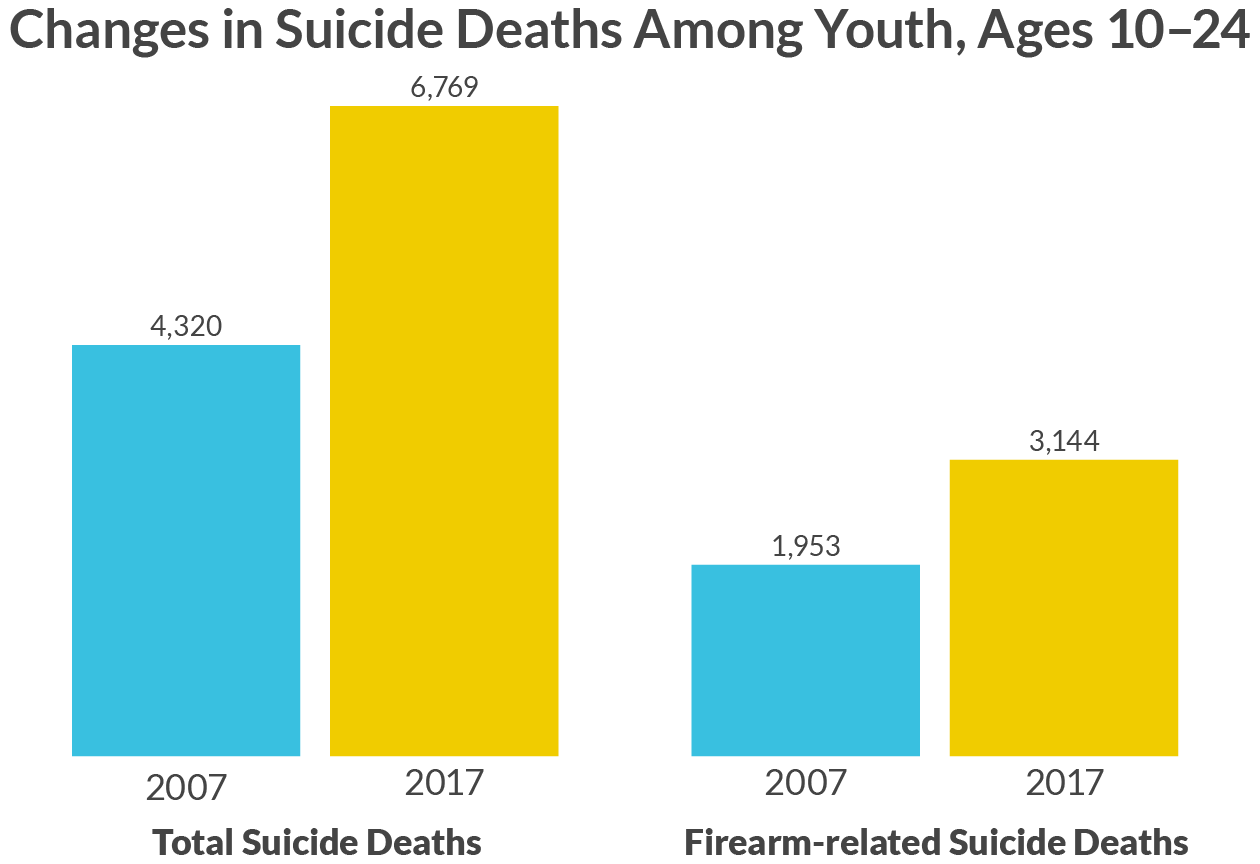
Between 2007 and 2017 there was a more than 60% increase in the number of suicide deaths by firearms among youth ages 10–24. The number of total suicide deaths among youth ages 10–24 and the number that were firearm-related have both increased every year between 2007–2017. Strikingly, the number of firearm-related suicides more than tripled between 2007 and 2017 for youth ages 10–14. Greater than 60% increases were found across each of the major U.S. census regions. Increases in suicide rates cannot be accounted for by population growth as there was only a 2% increase in the population of youth ages 10–24 between 2007 and 2017 (US Census Bureau, 2019).
Methodology
Data in this report are based on information from all death certificates filed in the 50 states and the District of Columbia. The CDC’s Web-Based Injury Statistics Query and Reporting System was used to compile National Vital Statistics data on annual suicide counts for youth ages 10–24. Suicide rates were examined by means and segmented by 5-year age groups (10–14, 15–19, and 20–24 years), race/ethnicity based, and U.S. Census regions (Northeast, South, Mid-West, and West). The cause-of-death lists are based on the International Classification of Diseases-10. Of note, suicide rates in the National Vital Statistics System are likely an underestimate of the actual prevalence because some suicides, particularly those resulting from overdoses, might be inappropriately counted as an accidental death or unintentional injury (Stone et al. , 2017).
Looking Ahead
The most recently available national data on deaths by suicide indicates firearms as the primary means involved in suicide deaths among youth. Further, total suicide deaths and firearm related suicide deaths are continuing to increase among youth ages 10–24. In order to achieve the goal of ending suicide among youth, there is a dire need for funding devoted to better understanding the causes of suicide and to the implementation of practices known to reduce suicide deaths. In line with our collaborative Model School District Policy on Suicide Prevention, The Trevor Project supports the evidence-based practice of lethal means safety counseling (Zalsman et al., 2016), which suggests limiting a youth’s access to mechanisms for carrying out a suicide attempt in times of crisis.
Additionally, there is currently a lack of systematic data collection on sexual orientation and gender identity (SOGI) at the time of death, which limits our understanding of the risks that lead to violent death among LGBT youth, a population more than four times as likely to attempt suicide compared to peers (Johns et al., 2019; Kann et al., 2018). For example, the aforementioned data was able to be segmented by means, census region of the U.S., age group, and race/ethnicity, but not sexual orientation or gender identity. Currently, The Trevor Project and other leading suicide prevention organizations are working to improve training and procedures on the collection of sexual orientation and gender identity as part of death investigations. Through the ongoing efforts of our research, education, advocacy, and crisis services programs The Trevor Project continually works towards a day when suicide is no longer a major cause of death for youth.
| ReferencesCenters for Disease Control and Prevention (2019). Web-based Injury Statistics Query and Reporting System (WISQARS) [Data tool]. Retrieved from https://webappa.cdc.gov/sasweb/ncipc/leadcause.html. Accessed on October 10, 2019.Conner A, Azrael D., Miller M. (2019). Suicide case-fatality rates in the United States, 2007 to 2014: A Nationwide population-based study. Annals of Internal Medicine, 171, 885–895.Johns MM, Lowry R, Andrzejewski J, et al. Transgender Identity and Experiences of Violence Victimization, Substance Use, Suicide Risk, and Sexual Risk Behaviors Among High School Students — 19 States and Large Urban School Districts, 2017. MMWR Morb Mortal Wkly Rep 2019;68:67–71.Kann, L., McManus, T., William, H., Shanklin, S., Flint, K., Queen, B., … Ethier, K. (2018). Youth Risk Behavior Surveillance — United States, 2017. MMWR Surveill Summ, 67(SS-8), 1–114.Morgan, E. R., Rowhani-Rahbar, A., Azrael, D., & Miller, M. (2018). Public perceptions of firearm-and non-firearm-related violent death in the United States: A national study. Annals of Internal Medicine, 169(10), 734-737.Shenassa, E. D., Catlin, S. N., & Buka, S. L. (2003). Lethality of firearms relative to other suicide methods: a population based study. Journal of Epidemiology & Community Health, 57(2), 120-124Stone, D. M., Holland, K. M., Bartholow, B., E. Logan, J., LiKamWa McIntosh, W., Trudeau, A., & Rockett, I. R. (2017). Deciphering suicide and other manners of death associated with drug intoxication: A Centers for Disease Control and Prevention consultation meeting summary. American Journal of Public Health, 107(8), 1233-1239.U.S. Census Bureau. (2019). American Community Survey Demographic and Housing 1-Year Estimates. Generated using American FactFinder. Available at: http://factfinder2.census.gov. Accessed on October 8, 2019.Zalsman, G., Hawton, K., Wasserman, D., van Heeringen, K., Arensman, E., Sarchiapone, M., … & Purebl, G. (2016). Suicide prevention strategies revisited: 10-year systematic review. The Lancet Psychiatry, 3(7), 646-659. |
For more information please contact: [email protected]
